
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
Original Article
- Metabolic Risk/Epidemiology
- A Composite Blood Biomarker Including AKR1B10 and Cytokeratin 18 for Progressive Types of Nonalcoholic Fatty Liver Disease
- Seung Joon Choi, Sungjin Yoon, Kyoung-Kon Kim, Doojin Kim, Hye Eun Lee, Kwang Gi Kim, Seung Kak Shin, Ie Byung Park, Seong Min Kim, Dae Ho Lee
- Received June 18, 2023 Accepted August 16, 2023 Published online February 1, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0189 [Epub ahead of print]
- 761 View
- 45 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
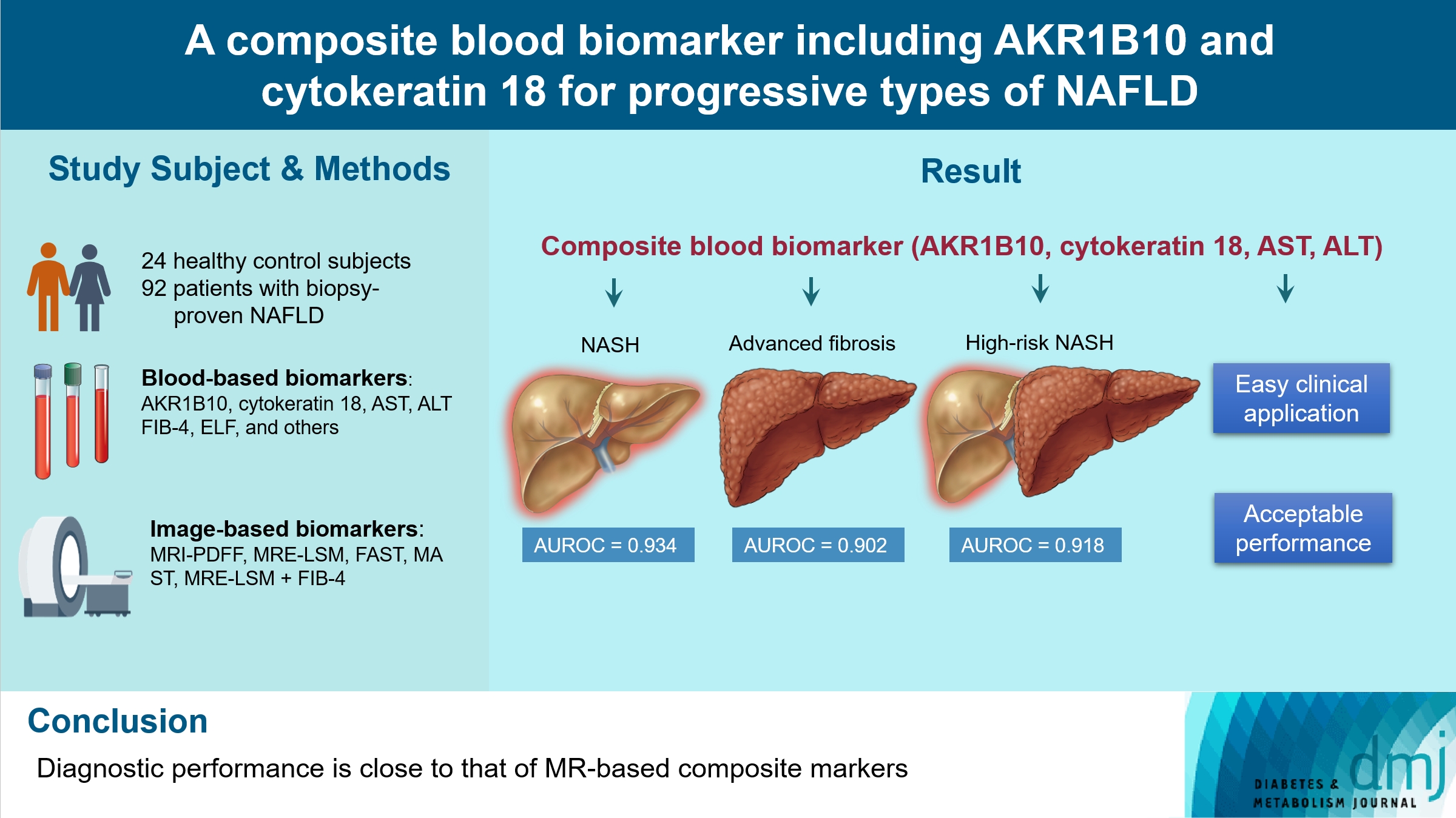
We aimed to evaluate whether composite blood biomarkers including aldo-keto reductase family 1 member B10 (AKR1B10) and cytokeratin 18 (CK-18; a nonalcoholic steatohepatitis [NASH] marker) have clinically applicable performance for the diagnosis of NASH, advanced liver fibrosis, and high-risk NASH (NASH+significant fibrosis).
Methods
A total of 116 subjects including healthy control subjects and patients with biopsy-proven nonalcoholic fatty liver disease (NAFLD) were analyzed to assess composite blood-based and imaging-based biomarkers either singly or in combination.
Results
A composite blood biomarker comprised of AKR1B10, CK-18, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) showed excellent performance for the diagnosis of, NASH, advanced fibrosis, and high-risk NASH, with area under the receiver operating characteristic curve values of 0.934 (95% confidence interval [CI], 0.888 to 0.981), 0.902 (95% CI, 0.832 to 0.971), and 0.918 (95% CI, 0.862 to 0.974), respectively. However, the performance of this blood composite biomarker was inferior to that various magnetic resonance (MR)-based composite biomarkers, such as proton density fat fraction/MR elastography- liver stiffness measurement (MRE-LSM)/ALT/AST for NASH, MRE-LSM+fibrosis-4 index for advanced fibrosis, and the known MR imaging-AST (MAST) score for high-risk NASH.
Conclusion
Our blood composite biomarker can be useful to distinguish progressive forms of NAFLD as an initial noninvasive test when MR-based tools are not available.
Review
- Guideline/Fact Sheet
- Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hypertension
- Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim, Committee of Clinical Practice Guidelines, Korean Society for the Study of Obesity (KSSO), Committee of Clinical Practice Guidelines and Committee of Food and Nutrition, Korean Diabetes Association (KDA), Policy Committee of Korean Society of Hypertension (KSH), Policy Development Committee of National Academy of Medicine of Korea (NAMOK)
- Diabetes Metab J. 2022;46(3):355-376. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0038
- 11,027 View
- 588 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
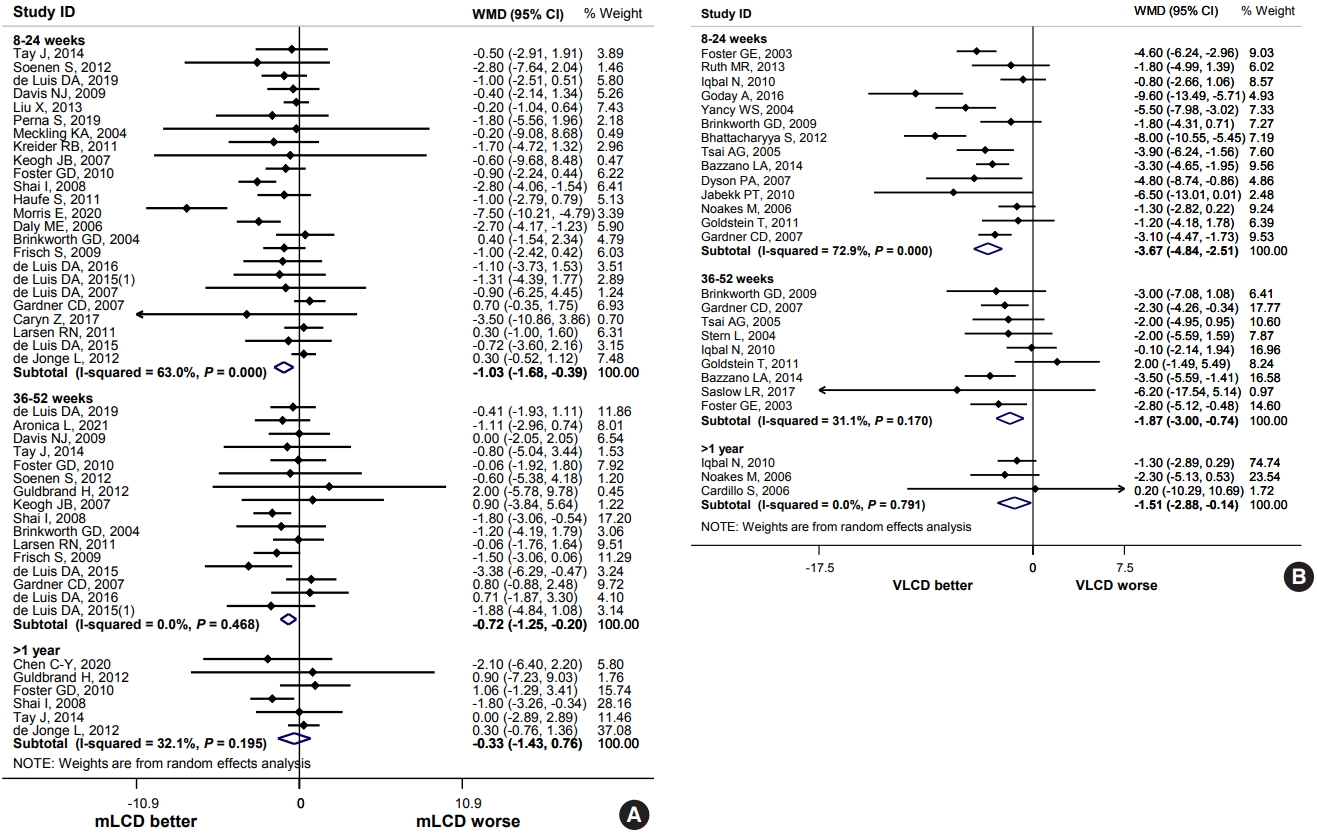
ePub - Carbohydrate-restricted diets and intermittent fasting (IF) have been rapidly gaining interest among the general population and patients with cardiometabolic disease, such as overweight or obesity, diabetes, and hypertension. However, there are limited expert recommendations for these dietary regimens. This study aimed to evaluate the level of scientific evidence on the benefits and harms of carbohydrate-restricted diets and IF to make responsible recommendations. A meta-analysis and systematic literature review of 66 articles on 50 randomized controlled trials (RCTs) of carbohydrate-restricted diets and 10 articles on eight RCTs of IF was performed. Based on the analysis, the following recommendations are suggested. In adults with overweight or obesity, a moderately-low carbohydrate or low carbohydrate diet (mLCD) can be considered as a dietary regimen for weight reduction. In adults with type 2 diabetes mellitus, mLCD can be considered as a dietary regimen for improving glycemic control and reducing body weight. In contrast, a very-low carbohydrate diet (VLCD) and IF are recommended against in patients with diabetes. Furthermore, no recommendations are suggested for VLCD and IF in adults with overweight or obesity, and carbohydrate-restricted diets and IF in patients with hypertension. Here, we describe the results of our analysis and the evidence for these recommendations.
-
Citations
Citations to this article as recorded by- Metabolic changes with intermittent fasting
Maria G. Lange, Alice A. Coffey, Paul C. Coleman, Thomas M. Barber, Thijs Van Rens, Oyinlola Oyebode, Sally Abbott, Petra Hanson
Journal of Human Nutrition and Dietetics.2024; 37(1): 256. CrossRef - Papel do Jejum Intermitente e da Dieta Restrita em Carboidratos na Prevenção de Doenças Cardiovasculares em Pacientes Pré-Diabéticos
Mohamed Khalfallah, Basma Elnagar, Shaimaa S. Soliman, Ahmad Eissa, Amany Allaithy
Arquivos Brasileiros de Cardiologia.2023;[Epub] CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef - Euglycemic diabetic ketoacidosis development in a patient with type 2 diabetes receiving a sodium-glucose cotransporter-2 inhibitor and a carbohydrate-restricted diet
Gwanpyo Koh, Jisun Bang, Soyeon Yoo, Sang Ah Lee
Journal of Medicine and Life Science.2023; 20(3): 126. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - The Related Metabolic Diseases and Treatments of Obesity
Ming Yang, Shuai Liu, Chunye Zhang
Healthcare.2022; 10(9): 1616. CrossRef - Updated Meta-Analysis of Studies from 2011 to 2021 Comparing the Effectiveness of Intermittent Energy Restriction and Continuous Energy Restriction
Kyoung-Kon Kim, Jee-Hyun Kang, Eun Mi Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(3): 230. CrossRef
- Metabolic changes with intermittent fasting

 KDA
KDA
 First
First Prev
Prev





